

Discover more from Dr. Christin Glorioso, MD PhD
Should you take metformin if you don't have diabetes?
How it works and the risk-benefit of taking it
Summary: I would not recommend taking metformin if you do not have diabetes because there is some evidence for, and a plausible mechanistic link to, increased risk of Alzheimer’s and Parkinson’s disease. Additionally, the evidence for beneficial metformin-induced lifespan extension in healthy animals is unconvincing and mixed.
Metformin, brand name Glucophage, meaning “glucose eater”, is a 1st line treatment for type II diabetes. Many people without diabetes are interested in taking it for potential lifespan extending properties. What does metformin do and should you take it?
What is metformin?
The biguanide class of antidiabetic medications originates from the French lilac or goat's rue (Galega officinalis), a plant used in folk medicine for several centuries. Metformin was first described in the scientific literature in 1922 as a product in the synthesis of N,N-dimethylguanidine. In 1929 its sugar-lowering action in rabbits was described. However, it wasn’t until 1972 that metformin was approved in Canada and 1994 in the U.S. (type 2 diabetes, Bristol-Myers Squibb). Generic formulations are now available in several countries, and metformin is believed to have become the world's most widely prescribed anti-diabetic medication.
How does it work?
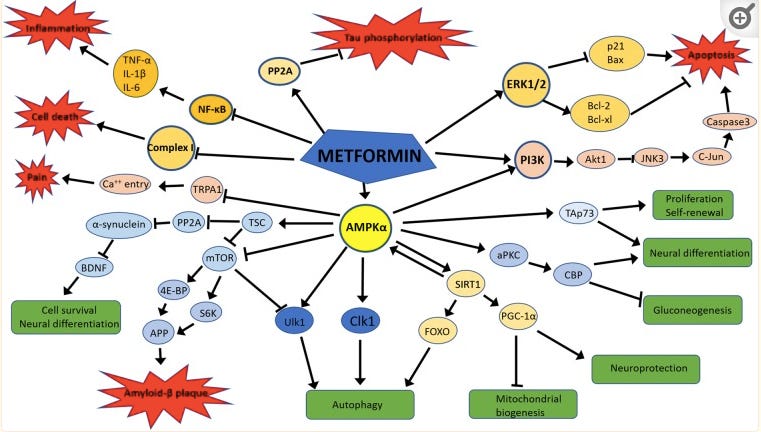
Metformin has multiple targets and its molecular mechanism of action is not completely understood. Amongst its most commonly cited mechanisms are inhibition of the mitochondrial respiratory chain (complex I), activation of AMP-activated protein kinase (AMPK), inhibition of cyclic adenosine monophosphate (cAMP), reduction of hepatic gluconeogenesis, and alteration of the gut microbiome. Additionally, metformin crosses the blood brain barrier making its effects on the brain relevant. Below are some of its proposed mechanisms of action in neurons and glia.
Does it extend lifespan?
Results are mixed on this in the animal literature. Some publications show that it extends lifespan in C. elegans and mice, some publications show that it is neutral with regards to or even reduces lifespan. Results depend on the species, sex, and genetic background of the particular animals used and the laboratory conditions under which it was tested. Metformin consistently shows no lifespan benefit in Drosophila (flies).
In humans there is a clear benefit to taking metformin for people who have type II diabetes. It improves glucose tolerance, is associated with weight loss, and decreases mortality— likely mediated through beneficial effects on diabetes. There are ongoing clinical trials to test metformin for anti-aging effects in humans with and without diabetes. The biggest ongoing trial is the Targeting Aging with Metformin (TAME) trial. The results from this study are not yet published.
Is metformin safe?
In the short-term it appears to be well tolerated. It has some side effects that are generally mild and related to GI upset. However, there is mounting evidence of metformin’s long-term potential to increase risk of neurodegenerative disorders including Alzheimer’s and Parkinson’s disease. From Kuan et al. (2017):
"We recruited 4651 patients in the metformin cohort and a comparable number of nonmetformin controls by using propensity score matching. Multivariate Cox proportional hazards regression was used to estimate the effects of metformin on the risk of dementia and PD after adjustment for several confounding factors. During the 12-year follow-up, the metformin cohort exhibited a higher risk of PD than the nonmetformin cohort (hazard ratio [HR]: 2.27, 95% confidence interval [CI]=1.68-3.07). The metformin cohort had an increased risk of all-cause dementia (HR: 1.66, 95% CI=1.35-2.04). Moreover, metformin exposure increased the risk of Alzheimer's disease (HR: 2.13, 95% CI=1.20-3.79) and vascular dementia (HR: 2.30, 95% CI=1.25-4.22)…Additional large-scale, prospective controlled trials are required to confirm the observed association in patients with T2DM.”
And from Koo et al (2019):
“rapid deterioration of Mini-Mental State Examination and Verbal Immediate Recall scores was more frequently found in the metformin-taking group, even after adjustment for age, sex, education level, baseline cognitive function, baseline glycated hemoglobin levels, renal and liver function, body mass index, hypertension, dyslipidemia, antidiabetic agents other than metformin, and baseline brain imaging abnormality (odds ratio 4.47, 95% confidence interval 1.24-16.05 and odds ratio 7.37, 95% confidence interval 1.19-45.56).”
While these individual level trials do appear damning for metformin in increasing Alzheimer’s and Parkinson’s risk, the gold standard for assessing clinical trials as a whole are meta-analyses— analysis of the analyses. I found only one such study on Pubmed “Association between metformin and neurodegenerative diseases of observational studies: systematic review and meta-analysis” from 2020. Here is what the authors found:
“In total, 23 comparisons out of 19 studies with 285 966 participants were included…Metformin was found to play a neutral role on the incidence of the overall NDs [Neurodegenerative Disorders]. Subgroup analysis showed metformin exposure increased the risk of Parkinson disease (PD) by 66% (OR 1.66, 95% CI 1.14 to 2.42).”
How might metformin be increasing risk of neurodegenerative disorders?
There are several important red flags amongst metformin’s mechanisms of action. The first is inhibition of mitochondrial complex I. There are two other drugs known to inhibit complex I and cause Parkinson’s disease— a pesticide, called Rotenone, which has been linked to increased incidence of PD in farm workers and the neurotoxin, MPTP. Complex I also decreases in expression with age in the human brain. This is opposite direction from age-related changes in mouse brain. This demonstrates the broader problems with translating rodent studies to human, particularly with regards to the brain, and may explain why aging biologists have largely failed to note the risks of metformin. From Oh et al 2011:
“the moderate transcriptome correlations and partial functional concordance between late-life human and rodent cohorts (13-77 years in humans and 3-24 months in mice) suggest limitations of the mouse to model normal aging of the human brain cortex.”
Another red flag in metformin’s mechanism is the decrease of Brain Derived Neurotrophic Factor (BDNF) associated with its use. BDNF is a growth factor for neurons and is induced by exercise and other neuroprotective strategies. It decreases with age. Metformin decreasing BDNF is a bad thing for the human brain. In fact there are ongoing clinical trials to increase BDNF in order to treat Alzheimer’s disease. From Chaudhari et al (2019):
“The decrease in BDNF suggests a potential state of vulnerability for the brain, as well as a decrease in neuroplasticity, which is necessary for enhanced cognitive effects. Long-term use of metformin reduces BDNF transcription and inhibits nuclear factor E2-related factor 2 (Nrf2), which may increase the vulnerability of the central nervous system. Some studies have also suggested that metformin increases the risk of PD or even aggravates neuronal damage.”
So what is the promise of metformin?
We need to untangle its many mechanisms of action and take the good ones and leave the bad ones. We can then create new drugs that preserve the helpful anti-diabetic properties while not potentially increasing the risk of neurodegenerative disorders. It may also be useful to create a version of metformin that does not cross the blood brain barrier in order to avoid the harmful effects on the brain while preserving the helpful effects on the rest of the body. In the meantime, I strongly advise against off-label use of metformin for anti-aging purposes because of the associated increased risk of neurodegenerative disorders.
If you want to know more about healthy aging and chat about this and other topics, you can follow me on Twitter and subscribe below.





Thanks for this. I was taking metformin for around a year, although not consistently but stopped a couple of months ago due to some concerns. This reinforces that decision. Looking forward to the results of the TAME trial but this isn't encouraging.
Thank you for this essay on metformin. Good science! May I please have a link to a copy of your CV?